COVID-19 Basic Immune Response
Just for clarification: SARS-2 is the virus that causes COVID-19. The current COVID-19 PCR test measures viral RNA. It does not measure our immune response to the virus.
Viral RNA is only found in blood with active viral infection (or for a short period of time after recovery). In fact, in theory, we should get two consecutive negative PCR tests before considering someone previously infected “non-infectious”. When someone recovers from COVID-19, the PCR shortly after becomes negative.
To determine past exposure to SARS-2 we use serologic tests, which measure our immune response to the virus. These tests, which require blood (serum) collection, are able to quantify specific IgM and IgG levels against SARS-2. So, SARS-2 IgM and IgG are antibodies that infected people produce during the course of the infection (Ig M first, followed by Ig G). These antibodies normally (in most other viral infections) are long-lasting, and could protect the body from future infection with the same virus.
Most anti-viral antibodies are protective, for example, hepatitis B IgG (or HBS Ab), which protects the body from HBV re-infection. Sometimes antibodies that the body produces after a viral infection can last for life but are not protective, such as the ones our body produces after a hepatitis C infection (thus we can get re-infected with HCV).
Currently, we can measure SARS-2 antibodies, but their utility to help in the diagnosis of acute infection or recovery are not better than the PCR. They can be used for epidemiological reasons (to find out the proportion of people already infected or susceptible).
They could potentially be used for treatment, using concentrated serum from people who recovered from the infection, to treat the acutely infected person. Think about it like the immunoglobulin shot some people get during an outbreak of hepatitis A. The validity of this approach for treatment of COVID-19 has not been well studied.
The ability of any anti-viral antibodies to protect a person later depends on various factors, such as:
- The antibody preferably needs to attach to a crucial viral part, making it unable to replicate. Sometimes the antibodies the body produces attach to a virus part that do not neutralize the virus.
- Our body needs to create a memory T-cell response that will recognize the virus later, after a future re-exposure.
- The viral surface glycoproteins, which are the sites where the antibodies attach, should not change much with time. In essence (although not quite), this is what happens after infection with the influenza virus.
It is unclear how long-lasting the antibodies produced by the body during COVID-19 are able to last or to protect the body in the future. There has been some case-reports of re-infection, which if true, it suggests that our body’s antibody production may not be fully protective after COVID-19.In reality, it is my understanding that this is yet to be elucidated.
If COVID-19 becomes a recurrent infection, SARS-2 serology tests may play a clinical role in the future. For the time being, we just don’t know yet.
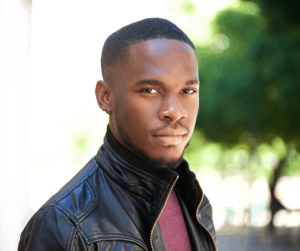
By Edwin DeJesus, MD, FACP, FIDSA
More Articles
Dr. DeJesus Recognized by Orlando Magazine
For the 5th consecutive year, Dr. DeJesus has been recognized by his peers in Orlando Magazine for his work as medical director at Orlando Immunology Center. Dr. DeJesus is a graduate from the University of Puerto Rico, School of Medicine. He completed his Internal Medicine training and Infectious Disease fellowship at the Medical College of…
Read MoreJoin OIC at the 2015 AIDS Walk Orlando
Orlando Immunology Center is pleased to announce that we will again be sponsoring a team at this year’s 2015 AIDS Walk Orlando. If you are interested in joining our team or donating to this worthwhile cause, please let us know. Saturday, March 28, 2015 In Florida, 15% of all new HIV infections reported among females…
Read MoreOIC Wins Wave Award for Favorite Local Healthcare Professional
The Orlando Immunology Center (OIC) announced today they have received the Central Florida/Orlando 2015 Watermark Awards for Variety and Excellence (WAVE) Award for favorite local healthcare professional. “We see this as a huge honor and will continue to do everything in our power to help patients from all walks of life be healthy, happy and…
Read More[NPR] How Safe Is It To Eat Takeout?
With the fear of infection on our minds these days, it’s easy to get panicky about everyday choices. Infectious disease and food safety experts weigh in on ordering dinner to-go. “I know people are worried, but from what we know currently about the virus, it’s safe to eat food prepared at restaurants so long as…
Read More[FactCheck] COVID-19 Face Mask Advice, Explained
It’s a seemingly simple question that has divided experts and nations since the beginning of the COVID-19 outbreak: Should members of the public who aren’t sick use face masks to limit the spread of the disease? For months, the Centers for Disease Control and Prevention maintained that the only people who needed to wear face…
Read MoreOIC is now conducting COVID-19 Treatment and Prevention studies in addition to other clinical research trials! Inquire below today!
Orlando Immunology Center (OIC) is proud to announce to the Central Florida community that our research center located at 1707 N Mills Avenue, Orlando, 32803 has been selected by the National Institutes of Health (NIH) in collaboration with the HIV Vaccine Trial Network (HVTN) to participate in one of the most promising COVID-19 vaccine studies sponsored by Oxford University and AstraZeneca. OIC…
Read MoreTips For Social Distancing, Quarantine, And Isolation During An Infectious Disease Outbreak
In the event of an infectious disease outbreak, local officials may require the public to take measures to limit and control the spread of the disease. This tip sheet provides information about social distancing, quarantine, and isolation. The government has the right to enforce federal and state laws related to public health if people within…
Read MoreWhy Creating an HIV Vaccine Matters Now
Sex. We all have sex. It’s natural. We might not talk about it but it’s literally how we all got here. When was the last time you had sex? In the last year? This brings us to why creating an HIV vaccine matters now more than ever. But I don’t have HIV, so why does…
Read MoreWhat is the Purpose of PrEP?
What is PrEP? How effective is PrEP? How long do I take PrEP before it works? What medications are taken during PrEP? Does PrEP have side effects? How do I get started? Is PrEP right for me? Preventing an HIV infection could be what saves your life, and thanks to drugs like pre-exposure prophylaxis (PrEP), HIV…
Read MoreHurricane Ian Closure
Our office will close at 12pm on Wednesday, September 28th and remain closed through Thursday, September 29th due to Hurricane Ian. We will resume seeing patients as soon as it is safe to do so. For updates, please check back here or give us a call. Stay safe!
Read MoreTropical Storm Nicole Closure
Due to tropical storm Nicole, our office will be closed on Thursday, November 10th. All patients with appointments scheduled for Thursday will be seen through a tele-health visit. Those with procedures scheduled may be rescheduled on Friday or early next week. Our team will be reaching out to you to provide more details. We will resume…
Read More2022 Holiday Hours
So that we may all enjoy the holidays, our office will be closed on the following days. Thursday, November 24th Friday, November 25th Monday, December 26th Monday, January 2nd
Read MoreCharlotte-Paige Rolle, M.D. and Federico Hinestrosa, M.D. featured on Spectrum News 13
Our very own Charlotte-Paige Rolle, M.D. and Federico Hinestrosa, M.D. appeared on Spectrum News 13 to discuss Orlando Immunology Center’s recent progress in the research of long-acting HIV medications. CHECK OUT THE FULL STORY
Read More